Risks associated with the use of HRT
At BMACS Clinic, we strongly advocate for Hormone Replacement Therapy (HRT). However, we acknowledge that HRT carries potential risks for certain women. Our aim is not to downplay these risks but rather to offer clear explanations and empower women to make informed choices regarding their health.
Life often involves balancing risks and benefits. Based on current knowledge and extensive research, it’s widely recognized that, for most women requiring HRT, the benefits outweigh the associated risks. Common advice suggests women should aim for the lowest effective HRT dose to manage symptoms for the shortest duration.
However, there’s no specific limit for HRT duration. For women experiencing ongoing symptoms, lifelong HRT might be suitable. These individuals benefit from ongoing monitoring, including regular mammograms, blood pressure checks, and comprehensive blood tests, ensuring a level of surveillance that women not on HRT may not receive.
It’s essential to note that risks from HRT differ for women under 50 (visit Premature Menopause Clinic London for more information).


Highlighted Risks of HRT
Breast Cancer:
Concerns about breast cancer are prevalent among women and healthcare professionals. An in-depth understanding of these risks is crucial.
For many women, the mention of “HRT” evokes immediate concerns about breast cancer. This apprehension extends to men and healthcare professionals, including general practitioners and Gynaecologists. This association often creates resistance to HRT – who wants to risk cancer with a treatment often perceived as a “lifestyle” choice?
However, the fact remains that life involves risks, some greater or more worthwhile than others. Therefore, it’s imperative to comprehend the extent of breast cancer risk linked to HRT for informed decision-making.
Based on established research
– Among 1000 women not on HRT, 23 may develop breast cancer over 5 years.
– Among 1000 women on HRT with estrogen and progesterone, 27 may develop breast cancer: an additional 4 women in 1000 on HRT.
– Among 1000 women on estrogen-only HRT (after a hysterectomy), there’s no observed increase in breast cancer; in fact, most studies indicate lower risk.
We refrain from judgment on whether an extra 4 women in 1000 developing breast cancer while on HRT pose an unacceptable or acceptable risk in the broader context of life. We trust each woman to weigh the risks versus HRT’s benefits.


For Clarity
– Women post-hysterectomy don’t require progestogen in their HRT. Evidence suggests progestogen in HRT might contribute to increased breast cancer risk. Women without a uterus taking estrogen-only HRT show no heightened breast cancer risk; published data even hints at a potentially reduced risk compared to non-HRT users. (We do NOT advocate estrogen-only HRT for preventing breast cancer in women without a uterus.)
– Women with a uterus can get similar breast cancer protection by using a Mirena coil. This coil administers progestogen locally, theoretically safeguarding against womb cancer without increasing breast cancer risk. However, research confirming reduced breast cancer risk with estrogen-only HRT and a Mirena coil is lacking.
– Some HRT specialists attempt to lower breast cancer risk from progestogens by administering them every 3-4 months to shed the womb lining, protecting the womb while minimizing progestogen exposure. However, there’s no conclusive evidence supporting this approach in reducing breast cancer risk.
Watch our informative videos on HRT and breast cancer – [HRT Breast Cancer](video link), [HRT Breast Cancer](video link).
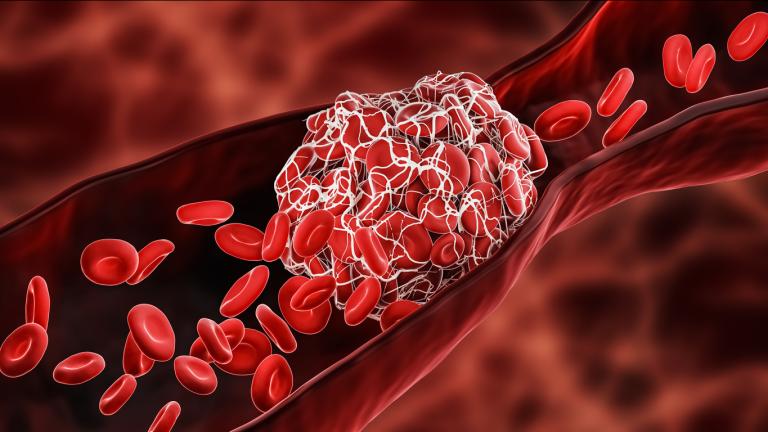
Venous Thromboembolism (VTE) - Blood Clotting
Oral HRT (estrogen and progesterone or estrogen-only) heightens the risk of blood clots and stroke. Studies indicate that the risk associated with HRT is notably lower than contraceptive pills or pregnancy. Transdermal estrogen (patches) appear safer regarding blood clot risk. At BMACS Clinic, we prefer transdermal over oral HRT unless specifically preferred by the patient. A history of blood clots or related complications is a relative contraindication to conventional HRT.
Stroke
Stroke
Stroke risk may increase with estrogen-only or combined HRT. However, this risk doesn’t significantly rise in women under 60. For instance, if 2 in 100 non-HRT users have a stroke, it might increase to 3 in 100 HRT users. Transdermal estrogen might associate with a lower stroke risk
Endometrial (Womb Lining) Cancer
Endometrial (Womb Lining) Cancer
Estrogen-only HRT escalates endometrial cancer risk in women with a uterus. Continuous combined HRT or cyclical progesterone eliminates this risk. Using a Mirena coil might safeguard against endometrial cancer, enabling estrogen use without additional progestogen, potentially reducing breast cancer risk.
Heart Disease
Heart Disease
Women over 60 using HRT more than 10 years post-menopause show a slight increase in heart disease risk. However, the risk itself is minimal. Over five years, nearly 2 in 100 women on HRT faced heart disease, compared to 1.5 in 100 women without HRT. Early commencement of HRT might minimize heart disease risks.
Other Risks
HRT use for a year or more might increase gallbladder disease risk. Data on HRT’s role in ovarian cancer risk is conflicting; some suggest a slight increase, diminishing upon stopping HRT
